Co-Production or Consultation? What Gloucestershire’s Maternity Papers Reveal — and Why True Collaboration Matters
꩜ Why I Care About Maternity Co-Production
I recently questioned Gloucestershire Maternity Services regarding claims that service users,
women and families are involved in co-production.
This is one way we can enact change in Maternity
-but it is not easy.
There are many women like me both inside and outside of the NHS trying to make things better
-here’s a bit about how I’ve tried,
-how Gloucestershire have tried
and where we are at now in Gloucestershire & the UK.
As I became a mother,
I was lucky to have received
exceptional care from an independent midwife,
It was incredibly transformational
Being honoured and supported throughout my journey meant everything to me
and I felt a deep sense of gratitude
for the means to be able to afford this care
(thanks to my late Gran!)
— and something else:
a determination that other women,
those without the privilege or means to pay privately,
should also have access to that same gold-standard,
one-to-one midwifery care.
My First
Service User Maternity Meeting
At the time,
the NCT (National Childbirth Trust)
spoke highly of
Maternity Services Liaison Committees
(now known as Maternity and Neonatal Voices Partnerships, or MNVPs).
NCT encouraged passionate parents to go along & get involved
— to take forward the ‘One Woman, One Midwife’ campaign —
brilliant I thought - and so off I went,
naively sure that my voice could make a difference.
But that first meeting shocked and changed something in me.
I was used to formal meetings in my work,
yet this clinic setting,
the horseshoe of tables,
the uniforms,
the hierarchy,
it all felt rather icy.
Yet still, I spoke.
And I remember the response word for word:
“Well, we have lots of Bangladeshi women here
— they don’t speak English, and they don’t want continuity.
And anyway, midwives don’t want to work like that.”
I was flabbergasted!
I was a new mum,
passionate but naïve,
and I was completely shut down.
I hadn’t expected it.
I didn’t yet understand
and was not prepared for the structures of the NHS maternity system
or the terms of reference for those committees.
But I didn’t give up.
I thought that if I just kept going
— if I kept showing up —
they would stop seeing me as a threat.
If I could prove I was on their side,
trying to improve things,
surely something would shift.
Years passed, and I continued attending meetings in Oldham & Rochdale later in Tameside,
and also Manchester
hopeful each time that change might finally come.
One particular moment stands out:
doulas in Manchester were invited to help choose colour schemes for the new Birth Centre.
After years of building relationships,
advocating for women,
and trying to open space for true co-production,
I found that request utterly insulting
a stark reminder that what we were being offered wasn’t partnership,
just tokenism 😭
That was the moment I realised these meetings were never meant to be co-production.
They were, at best, an engagement theatre
— a tick-box exercise,
a distraction that wasted everyone’s time: mine, theirs,
and the other birthworkers and service users
who kept showing up hoping for something more.
It doesn’t mean those people weren’t good at their jobs,
or that they didn’t care about women.
They absolutely did.
But the defensiveness that permeated those spaces wasn’t personal
— it was cultural.
It’s a symptom of the system of blame within the NHS,
where genuine openness can feel unsafe.
Now I understand differently.
It is not for us
— for service users, teacher, doulas, or community advocates —
to prove ourselves worthy of co-production.
Because we cannot overcome this culture of fear,
by asking politely.
It is for us to speak up and demand it,
as a legal and ethical responsibility,
and to call it out when it is not happening.
Defensiveness, lip service and tokensim
have no place in improvement work
— it is counterproductive and costly
to the overall cause of women’s health.
Thankfully, I have since witnessed moments where genuine collaboration is possible
— where professionals and community voices sit as equals, share responsibility,
and make real change together.
But those moments remain far too rare.
🌼 From Personal Experience
to Public Inquiry
Over the past 18 months
— after taking a “birth-work sabbatical” —
and settling here around 5 years ago
I began quietly exploring maternity care in the Forest of Dean.
I’ve been speaking with and supporting local parents,
both before and after birth, and have attended births in the area too.
It quickly became clear that something fundamental was missing.
The new hospital was built without any maternity services,
despite earlier promises of an ultrasound unit
(as noted in the meeting minutes below).
At the same time, a familiar story was emerging.
Gloucester Royal Hospital was once again deemed unsafe following inspection.
Many women I spoke with said
they’d been told by midwives there
wasn’t enough capacity to support home births,
and I have yet to meet a single woman
who had a known midwife during labour or birth.
And yet — there is hope….
A new Maternity Transformation Project is underway,
and a new MNVP team is being recruited,
more midwives have been drafted in.
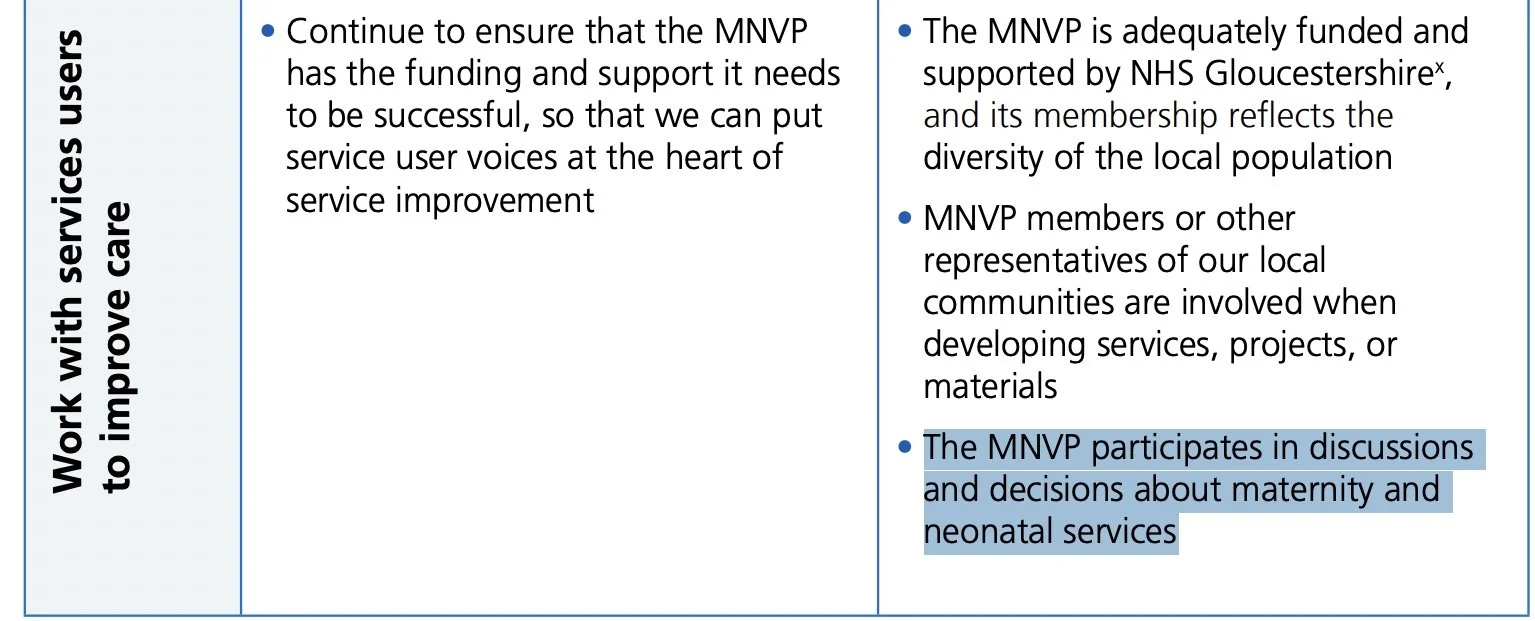
Gloucestershire NHS publicly state that they are
woking with MNVP to develop their new maternity plan
fOR families and communities.
(The FOR is important too we will come back to that later…)
Curious to see what that all this really meant in practice,
I submitted a Freedom of Information (FOI)
request asking for evidence of the co-design taking place.
The response?
The documents at the bottom of the page.
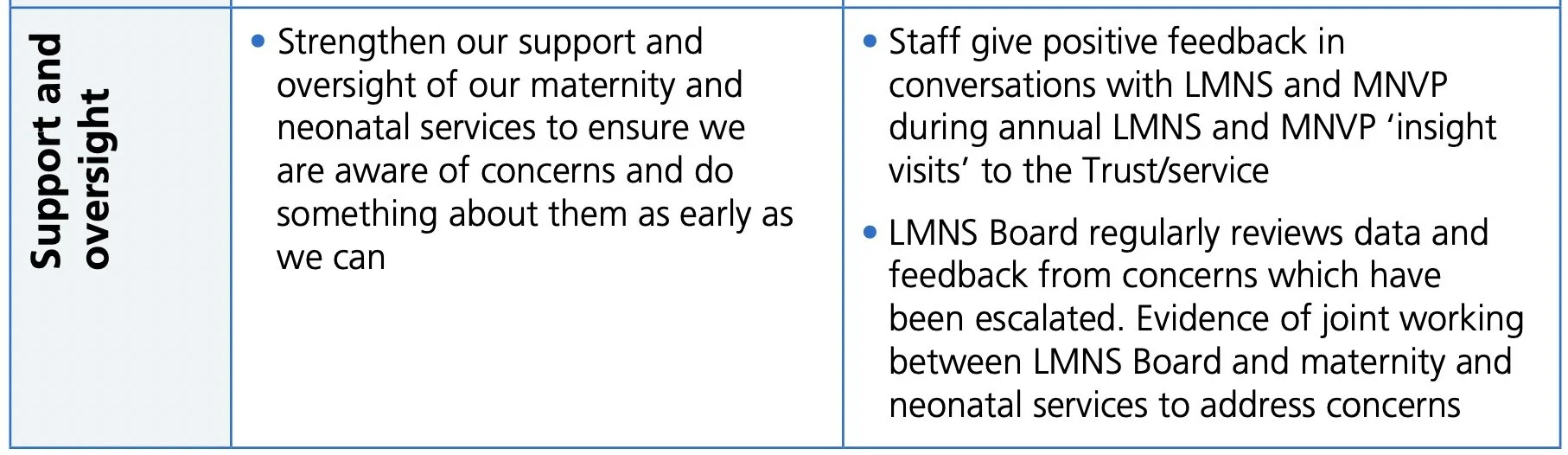
🔍 What the Documents Revealed
On an initial analysis - these minutes & registers
one thing stood out clearly
— there are plenty of good examples of:
information gathering, listening and sharing,
but none of true co-production or shared decision making
It isn’t easy to achieve genuine co-production.
It takes willingness, dedication on both sides,
and most importantly,
a shared understanding of what co-production actually looks like in practice.
So, in the next part of this article,
I’ll explore — for the purposes of education
and for anyone interested in maternity quality improvement
— exactly what co-production means,
what it doesn’t,
and how we can move towards doing it well.
🌱 What Co-Production Really Means
“Co-production is not just a word, it is not just a concept,
it is a meeting of minds coming together to find shared solutions.In practice, co-production involves people who use services being consulted, included,
and working together
from the start to the end of any project that affects them.When co-production works best,
people who use services and carers are valued by organisations as equal partners, can share power and have influence over decisions made.”
— Think Local Act Personal, cited by The King’s Fund
Alongside NHS England’s own description in its Co-Production and Quality Improvement: A Resource Guide:
“Co-production means designing services with people,
not for them.
It requires sharing power,
responsibility and decision-making equally
between people who use services and those who provide them.”
Together, these definitions remind us that co-production isn’t a buzzword or a single event — it’s a relationship. It’s built on trust, transparency and equal footing.
When it’s done well, decisions are made together,
and people with lived experience are recognised as experts in their own right.
🕊️ When It Works
Having helped co-create a Post-Dates Leaflet with the Bath MNVP last year,
I’ve seen what genuine co-production looks like.
It was collaborative from the start
— midwives, doulas, antenatal teachers and local mothers sitting together,
listening to each other’s experiences,
shaping wording,
tone and imagery
until everyone felt it reflected both clinical accuracy and lived reality.
That process didn’t just produce a leaflet; it built understanding and trust.
Everyone left feeling heard and valued
— which is exactly what true co-production is meant to achieve.
Caveat - ALL leaflets should be written at top level with service user collaboration
rather than each trust wasting time re-inventing the wheel.
But having said that it was a very small good example
and I was pleased to have been a part of it.
⚙️ When It Doesn’t
By contrast, what we often see
(including in some of the Gloucestershire documents released under FOI)
is consultation dressed up as co-design or user involvement...
Families are invited to
“share their views,” presentations are made
but decisions are made elsewhere, regardless.
Listening sessions and coffee mornings are counted as “collaboration,”
but there’s no record of shared decision-making or evidence that feedback changed anything.
This is what The King’s Fund calls “engagement theatre”
— where the appearance of listening replaces the practice of partnership.
🌿 Why It’s So Hard to Do Well
It’s not always bad faith.
There are real barriers that make co-production difficult to achieve:
Lack of understanding
Many professionals believe inviting feedback = co-production,
but it’s a different level of partnership entirely.
Time and capacity
Genuine collaboration takes time
— and overstretched maternity staff are rarely given protected hours to do this properly.
Funding and resources
Paying service users for their time,
training facilitators,
or covering travel and childcare requires budget
— often missing.
Fear of criticism
In a system under pressure,
honest feedback can feel threatening rather than useful.
Power imbalance
Without clear structures, professionals still hold the final say
— which undermines equal partnership.
Short-term leadership
MVP leads and engagement roles are often part-time or temporary,
breaking continuity.
Defensiveness and hierarchy
Staff feel watched or judged,
service users feel tokenised,
and the space for open dialogue closes.
Acknowledging these barriers doesn’t excuse them
— but it does help us understand why so many
“co-design / user-involvement”
claims don’t hold up under scrutiny.
🌻 How We Move Forward
Real co-production begins with a shift in mindset: from consulting to sharing control.
Here are a few ways local systems could start closing that gap:
Train both staff and service users in what co-production really means — and how to do it safely.
Pay and support lived-experience partners as equal contributors, not unpaid volunteers.
Build continuity — stable MNVP leadership, consistent meeting attendance, and transparent action tracking.
Publish evidence of influence — clear minutes showing what feedback changed.
Create independent spaces (like listening circles) facilitated by community partners rather than the NHS itself.
Embrace humility — co-production requires letting go of control to create something better together.
🌼 Why I’m Sharing This
I share these experiences for both service users and professionals,
because the Maternity and Neonatal Voices Partnerships are still being funded,
and people are still giving their time.
If we’re going to do this, let’s do it well.
Perhaps our first role
— whether as a lay member, a professional, or a volunteer
— is education: whether that’s for ourselves or collectively as a group.
Understanding what true co-production actually is,
what it looks like,
what’s expected,
and recognising the ways it can and does work when everyone is on board.
It is my greatest wish that we stop wasting our time
— and the NHS’s resources
— on lip service and tokenism.
If funding is being invested,
and if legislation clearly requires co-production,
then let’s make it happen
— for the benefit of birthing women,
and for the families and communities
who feel the ripple effects of those experiences for years to come.
So I invite you to explore the links and case studies below,
and to look through the documents released by Gloucestershire.
Familiarise yourself with maternity policy,
human rights law,
and the national frameworks that define what co-production really means
— because awareness is the first step to accountability.
Together, we can raise the standard
— not just for reports and reviews, but for the real,
lived experiences of women, babies, and families across the UK.
📚 Further Reading & Resources
If you’d like to understand more about co-production, maternity transformation, and the rights of women and families in maternity care, these are some of the most useful national resources to explore:
🏥 Co-Production & Maternity Policy
NHS England (2023) — Maternity and Neonatal Voices Partnership Guidance
NHS England (2023) — Co-Production and Quality Improvement: A Resource Guide
NHS England (2022) — Working in Partnership with People and Communities: Statutory Guidance (PDF)
Full list of Maternity Policy Documents since 2016 here.
🌿 Understanding Genuine Co-Production
The King’s Fund (2022) — How does the health and care system hear from people and communities?
Social Care Institute for Excellence (SCIE) — Co-production: what it is and how to do it
Coproduction Collective (UCL) — Case Study Examples of Co-Production in Action
⚖️ Rights & Accountability
Birthrights — Human Rights in Maternity Care
NICE — Community Engagement: Improving Health and Wellbeing
AIMS - Association for Improvements in Midwifery
Freedom of Information Findings: What the Papers Show
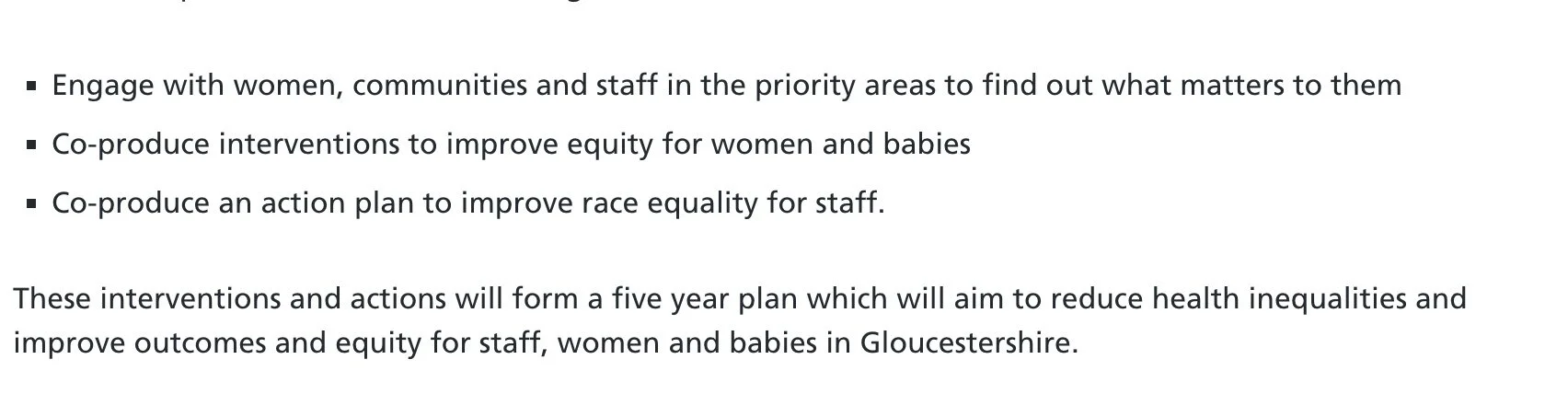
These documents were released following my Freedom of Information (FOI) requests to both the Gloucestershire Integrated Care Board (ICB) — the commissioners — and the Gloucestershire Hospitals NHS Foundation Trust.
The requests sought evidence of co-production in local maternity service development and examples of how women and service users had been placed at the centre of decision-making.
The response was revealing:
The Hospital Trust confirmed that it holds no evidence of co-production.
The documents provided instead came from the Integrated Care Board,
which commissions the Maternity and Neonatal Voices Partnership (MNVP)
— the group intended to represent service-user voices in planning and improvement.
Doula Coffee Mornings, Hosted at Gloucestershire Hospital
To make sense of what was released, I’ve grouped the documents into themes — starting with the “Doula Coffee Mornings.”
These gatherings were described as informal discussions aimed at fostering understanding between doulas and midwives. The conversations themselves were interesting — often centred on educating midwives about the role of doulas and the type of support they offer.
While this kind of relationship-building can be valuable, it’s important to note that these meetings were not examples of co-production. They were not advertised as collaborative planning sessions, and there was no agenda, structure, or record of shared decision-making.
It’s worth recognising, too, the time and personal investment made by doulas who attended — often unpaid, travelling into the hospital and paying for parking — in the hope that building bridges would lead to better understanding and smoother collaboration in practice.
Many women choose to hire doulas precisely because continuity within NHS maternity services is no longer guaranteed. They want consistent, trusted support throughout pregnancy and birth — something that should be standard, not a privilege.
Perhaps the real opportunity here lies in creating a culture where midwives and doulas can work alongside each other with mutual respect, acknowledging that both share the same goal: safer, calmer, more supported births.
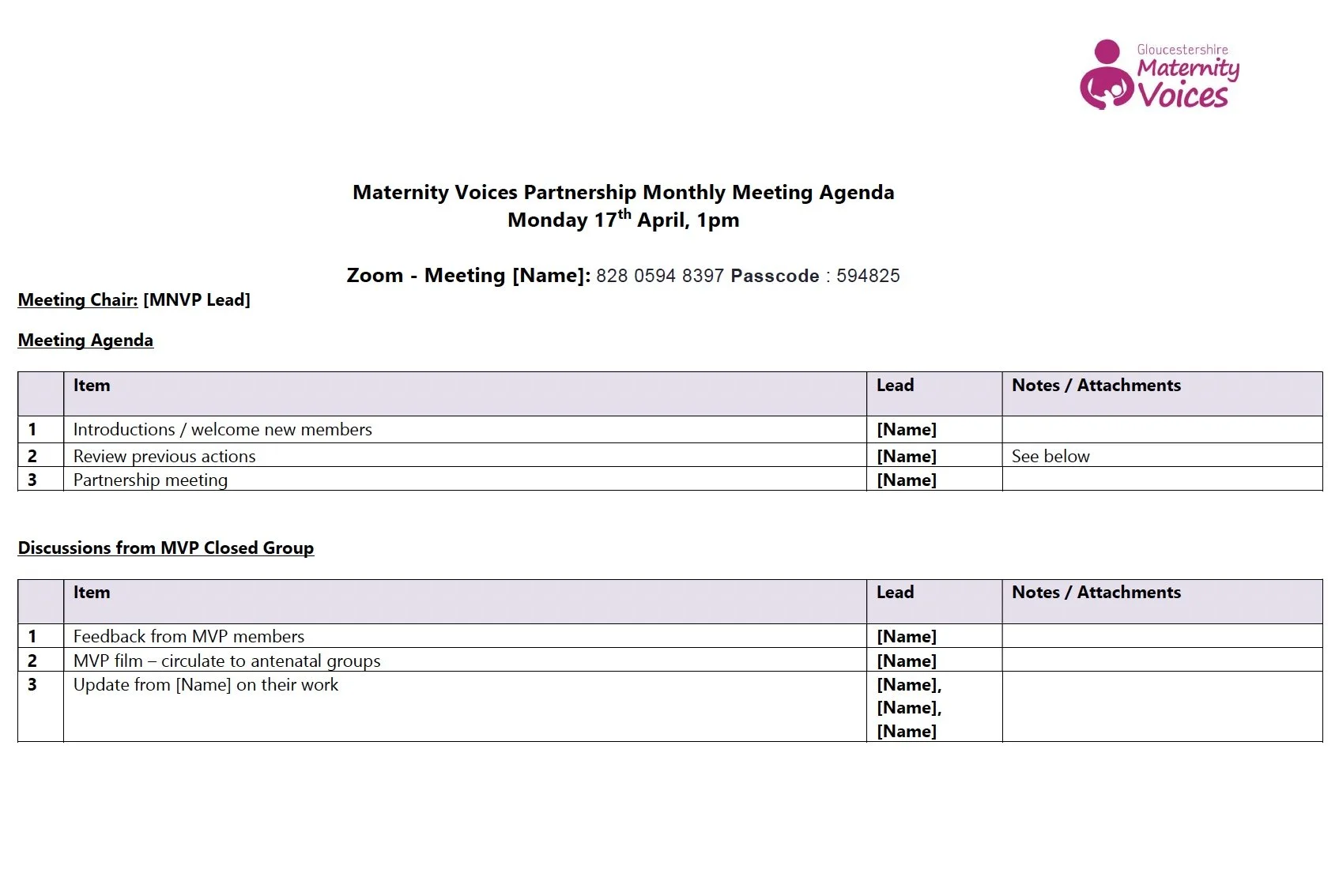
Maternity Voices Partnership – Monthly Meetings
The next set of documents relates to the Maternity and Neonatal Voices Partnership (MNVP) monthly meetings. I’ve tried to put them in chronological order, but this was far from straightforward. The files were inconsistently named, and several months appear to be missing entirely. In some cases, only an agenda was provided, with no minutes or action log attached.
Across all of the material, there is no clear record of who attended — the names and roles of participants (midwives, neonatal staff, health visitors, consultants, heads of midwifery, or service users) have all been redacted. This makes it impossible to see whether the meetings were balanced, representative, or attended by those with authority to act on the issues raised.
There is no evidence of agreed actions, follow-up dates, or Terms of Reference. Without these, it is difficult to establish what the group’s formal remit actually is — whether it functions as a decision-making body, a discussion forum, or simply a communications channel between the Trust and service users.
From what can be seen, the meetings seem to serve more as informal catch-ups or information-sharing sessions rather than spaces for collaborative planning or co-production. There is no indication of pre-reading being circulated, background data being shared, or progress being reviewed from previous meetings.
While information exchange has value, the absence of a clear structure or accountability framework raises questions about how service-user feedback is captured, prioritised, and turned into tangible improvements.
If the MNVP is intended to be the primary mechanism for women and families to influence local maternity care, then these records suggest that it currently lacks the consistency, transparency, and follow-through necessary to achieve that goal.
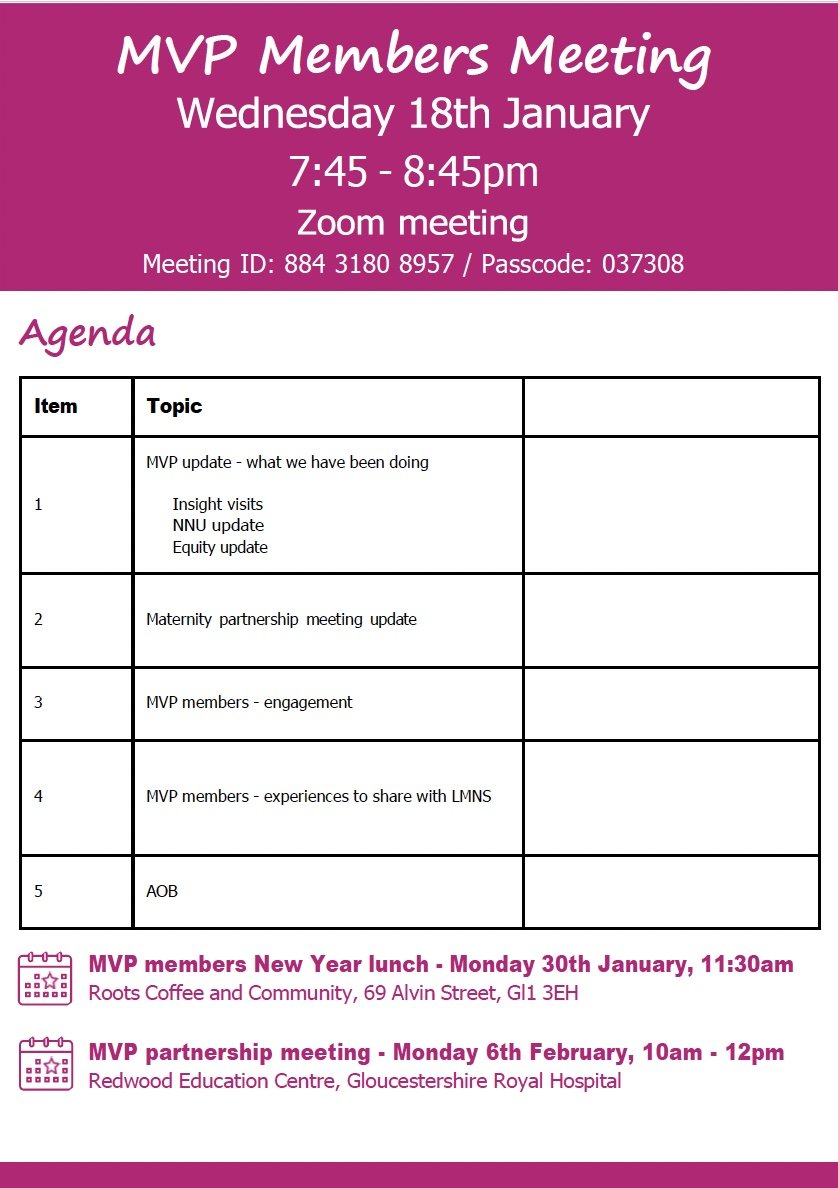
Maternity Voices Partnership Monthly Meeting Minutes
Wednesday 18th January 2023
Zoom Call – Recorded (all agreed to recording)
Evidence mainly of information sharing, rather than joint planning.
Discussion focused on how to engage members, suggesting difficulties maintaining consistent participation.
Reference to Dad’s Matter producing posters for the hospital – raises questions about policy on promoting external organisations within NHS premises.
No evidence of collaboration or shared decision-making recorded.
No Monthly Meetings for February & March
Or if there were - they were not recorded / minuted - no agenda…
Maternity Voices Partnership Monthly Meeting Minutes
Monday 17th April 2023
Zoom Call
This was the only record provided for that period — no additional minutes or attendance details.
Notes mention “reviewing actions” but give no indication of what those actions were, who was responsible, or whether any progress was made.
Time was spent watching a film that could be used in antenatal classes.
No evidence of collaboration or co-design with service users or community partners.
I’ve grouped those early MNVP meetings together because there was so little substance in the material provided.
Notably, there was no mention or discussion of the upcoming Partnership (Listening) Events, which began soon afterwards.
From a co-production perspective, this is puzzling.
One would expect these larger engagement sessions to have been planned, shaped, and reviewed through the MNVP — including discussion of how data would be collected, analysed, and acted upon.
As it stands, there is no clear indication of who initiated or organised the Partnership Events, or how the information gathered from them was intended to feed back into service design and improvement.
Partnership Meetings
The next group of documents covers a series of Partnership or “Listening” Events,
which brought together focus groups on a range of maternity-related topics.
Listening events can play an important role within a co-design process
— they provide opportunities to gather experiences, build understanding, and identify themes for improvement.
However, on their own, they do not constitute co-production or genuine user involvement.
In fact, social research shows that consultation exercises can sometimes create a false sense of participation:
when people are asked for their opinions,
they often feel included and are more likely to accept decisions
— even if those decisions remain unchanged.
These Gloucestershire events appear to have been well organised and presented,
yet there is no evidence of follow-up or documented action arising from them.
Without clear next steps, feedback loops, or outcomes,
it is difficult to see what these sessions achieved beyond giving an impression of listening
— especially troubling at a time when local maternity services are being reduced or centralised.
All Reports begin with:
The purpose of these events is to bring everyone together, to discuss the current situation within maternity care, listen to feedback about women and birthing peoples experience and coproduce ideas and solutions, which can be taken away as actions to improve the service.
This report notes the discussions and ideas from the focus groups.
These will now be discussed at the Maternity Experience Subgroup follow up meeting, to agree actions to take forward.
February -2023
Redwood Education Centre
2nd Partnership Group
Focus Groups
- Staff morale, care compassion
- Listening & Consent
- Feeding Support
- Waiting area for caesarean & induction
*There is an induction QI project in progress The MVP have sent all the feedback we have received about inductions to the QI project manager. We look forward to an update about how this feedback will be used to inform the project.
May-2023
Longford Village Hall
3rd Partnership Group
Maternity Strategy
[Name] updated the group about some of the work which has been going on to develop a maternity strategy. The three year delivery plan will also now feed into this.
Focus Groups
Feeling alone
Food and fluids
Shared decision making
Listening to women and birthing people with compassion
25th September ‘ 23
St Mark’s Church Hall, Church Road, Cheltenham
4th Partnership Group
Focus Groups
Communication between midwives & Health Visitors for vulnerable families
Home Labour Assessment
Pregnancy after Loss Support
If any Maternity Experience Subgroup follow-up meetings were held to review these Listening Events and agree actions, no records were shared in response to my request.
It’s also notable that no MNVP monthly meeting minutes appear between April and September 2023.
Whether these meetings were missed, unminuted, or withheld is unclear — but the next available record resumes in September 2023.
Maternity Voices Partnership Monthly Meeting Minutes
Monday 12th September, 10:30-11:30 am
Zoom Call – Recorded (all agreed to recording)
September 2023 MNVP meeting – Discussion points:
Health Visitors: Discussion centred on how Health Visitors could improve communication with women and families. It’s unclear why this topic was addressed within the MNVP rather than through dedicated Health Visiting meetings — raising questions about the group’s focus and purpose.
Social Media: Plans to “let everyone know there has been no progress” and to create a new group to improve engagement — effectively, a meeting about setting up more meetings.
Breastfeeding graphs: Ongoing work mentioned on producing breastfeeding data visuals — a task that has apparently continued since earlier meetings. It’s worth noting that the NHS Trust already receives a specific budget for breastfeeding support, making it unclear why this is being handled informally through MNVP discussions.
Engagement report: Primarily information sharing from Gloucestershire Maternity Services rather than a two-way process. Members were informed of developments but no feedback or collaboration was requested or recorded — raising the question of whether being told equates to being involved.
Next 3 Listening Events Commence
All reports start with this wording…
The purpose of these events is to bring everyone together, discuss the current situation within maternity care, listen to feedback about women and birthing people’s experiences and co-produce ideas and solutions. These can then be taken away as actions to improve services.
This report notes the discussions and ideas from the focus groups.
These will now be discussed at the Maternity Experience Subgroup follow up meeting, to agree actions to take forward
December 2023
Hilltop Children’s Centre, Cinderford
We were really pleased to welcome everyone to this event. We had 12 service users attend, along with some babies and toddlers. 6 representatives from community groups and 15 health professionals, including midwives and health visitors, also attended. In total we had 33 adults.
Presentations:
Neonatal Care
Maternity Scans
Focus Groups
Antenatal Education (what do people want from their classes)
Tour of the units
Experiences of Gloucester Hospital Triage
The consultant midwife gave an update stating that once the new Forest of Dean Community Hospital opened, it would provide dating, nuchal, and anomaly scans every Thursday. This news was warmly received at the time — families repeatedly said they wanted more local access to basic maternity services, given the travel barriers, parking costs, and lack of public transport to Gloucester.
However, as of November 2025, none of this has materialised.
There is no scanning clinic in the new hospital.
Antenatal classes remain virtually non-existent.
And feedback about Gloucester’s triage system continues to paint a bleak picture — many parents describing experiences that fall far short of what safe, compassionate care should feel like.
There was no follow-up or published feedback from this event — only the report itself, which now seems to serve more as evidence that consultation took place than as proof that anything changed.
It’s hard not to question whether these sessions were truly intended to drive improvement, or simply to create the appearance of listening — a paper trail of “engagement” without accountability.
12th June 2024
The Friendship Café, Painswick Road
We were very excited to welcome everyone to this event, anticipating such a large turnout: we had 22 service users attend (along with some babies and toddlers) and 3 representatives from community groups, representing the voice of service users. 24 NHS/public health professionals, including midwives, GPsand health visitors, also attended. In total we had 49 adults
Focus groups
Consultant Appointments
Scanning Clinics
Timings of Appointments & Cancellations
Booking Appointments
Neonatal Feeding
Personalised Care
Interesting discussions and action points from this well attended meeting. However, there is no evidence that any of these actions have since been implemented, tracked, or even revisited in later meetings.
Without visible follow-up, these detailed reports risk becoming archives of unfulfilled intentions — documents that look impressive on paper but fail to deliver change for the families whose experiences informed them.
22 October 2024
The Wheatpieces Community Group
Partnership Event no.???
We were pleased to welcome six service users to this event, alongside seven community group representatives and ten NHS and Public Health staff members.
Focus Groups
Martha’s Rule
Care Plans & Badger Notes
Health Visiting and Children’s Centre’s
Open Table
One of the focus groups discussed how consultants were being encouraged to use the BRAIN acronym (Benefits, Risks, Alternatives, Intuition, Nothing) to support informed decision-making with women.
This is a welcome step in principle — yet, as with many of the issues repeatedly raised in these forums, there is no evidence of implementation or follow-up.
It raises the broader question: How many times must the same feedback be heard before it leads to meaningful change?
Again and again, these reports highlight the same themes — communication gaps, rushed appointments, and women feeling unheard.
Continuity of care could resolve many of these problems, yet it remains largely absent from local service models.
Without continuity, every “listening” event risks becoming a repeat performance — new venues, familiar faces, and the same unmet promises.
Missing Follow-Up and Final Documents
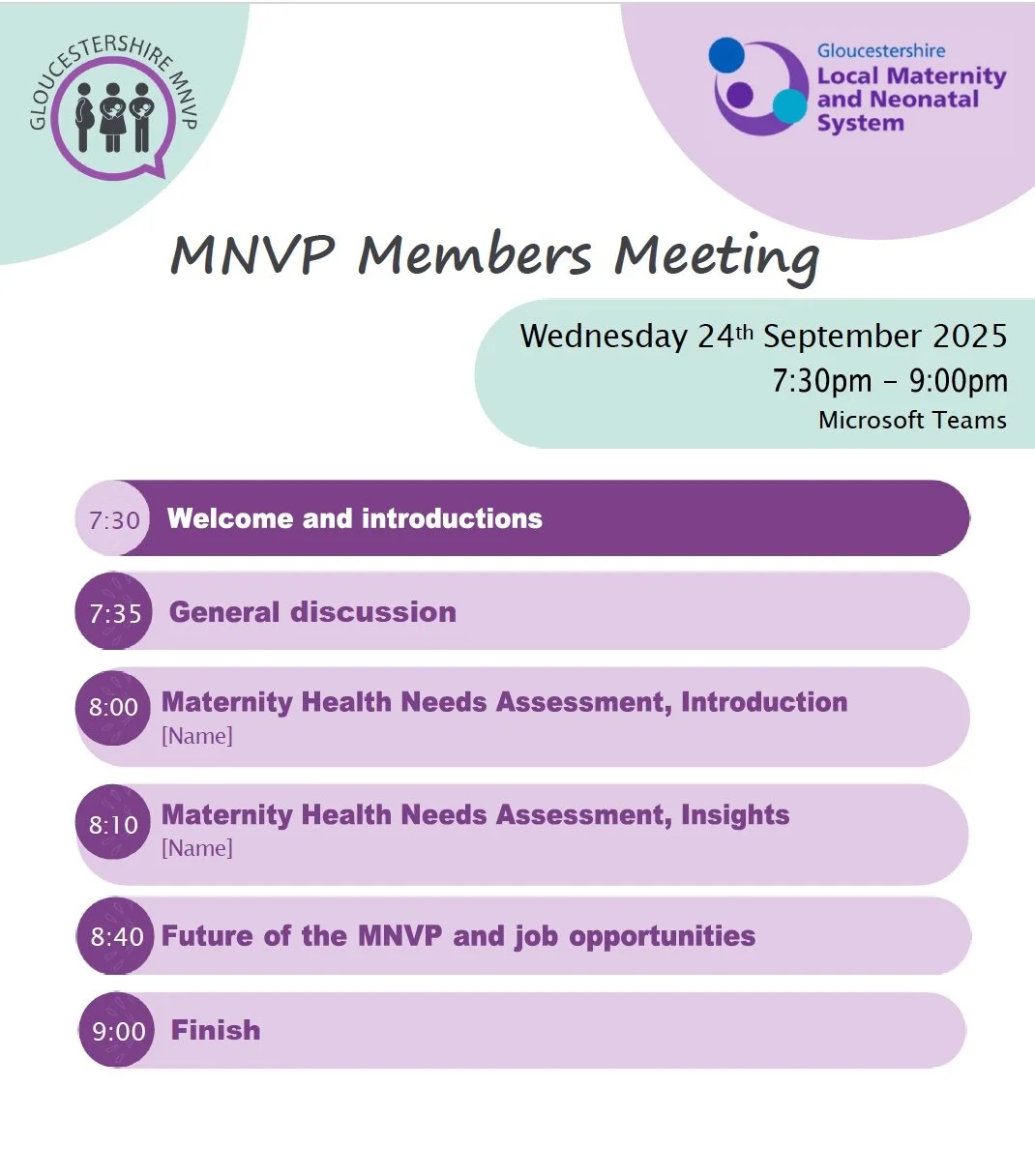
After October 2024, no further follow-up reports or MNVP meeting minutes were provided.
The only additional materials included were a handful of posters promoting Partnership Events,
one of which appears to relate to a September 2025 meeting
— yet there are no accompanying minutes or evidence of discussion.
If these documents represent the best examples of user involvement that were available,
it raises serious concerns about what has not been shared
— or perhaps, what has not taken place.
There were also three sets of Neonatal Bereavement meeting notes included in the FOI response,
each with its own scope and terms of reference.
These followed a similar pattern to the MNVP meetings
— largely information sharing and updates
— so I have chosen not to analyse them in detail for this article.
Overall Reflections
Taken together, these documents paint a picture of activity without accountability. Meetings were held, events were hosted, and reports were written — yet there is little to no evidence that any of it resulted in measurable change, co-authored decisions, or lasting improvement for women and families in Gloucestershire.
The language of co-production appears frequently — in mission statements, introductions, and templates — but the practice itself is absent. What emerges instead is a pattern of consultation: opportunities for people to speak, but not to shape.
True co-production requires transparency, continuity, and shared power. None of these can exist without clear documentation, follow-up, and a willingness to act on feedback — qualities missing from the material provided under this Freedom of Information request.
This analysis is not written to criticise individuals, but to highlight a structural problem. When “listening” becomes a substitute for change, trust is lost — and with it, the very foundation of safe, compassionate maternity care.