Low PAPP-A: What It Really Means and How to Support Your Placenta Naturally
If you’ve been told you have low PAPP-A,
you might have felt that sinking worry
— as if your body has done something wrong.
Often, women are told this means their placenta
“isn’t working properly”,
that they’ll need more scans,
and sometimes that they’ll have to be induced.
But let’s pause for a moment.
Low PAPP-A isn’t a diagnosis — it’s a marker and a snapshot.
It tells us that your placenta might need a little extra love and attention.
And there is so much you can do to support that naturally.
🌸 What Is PAPP-A?
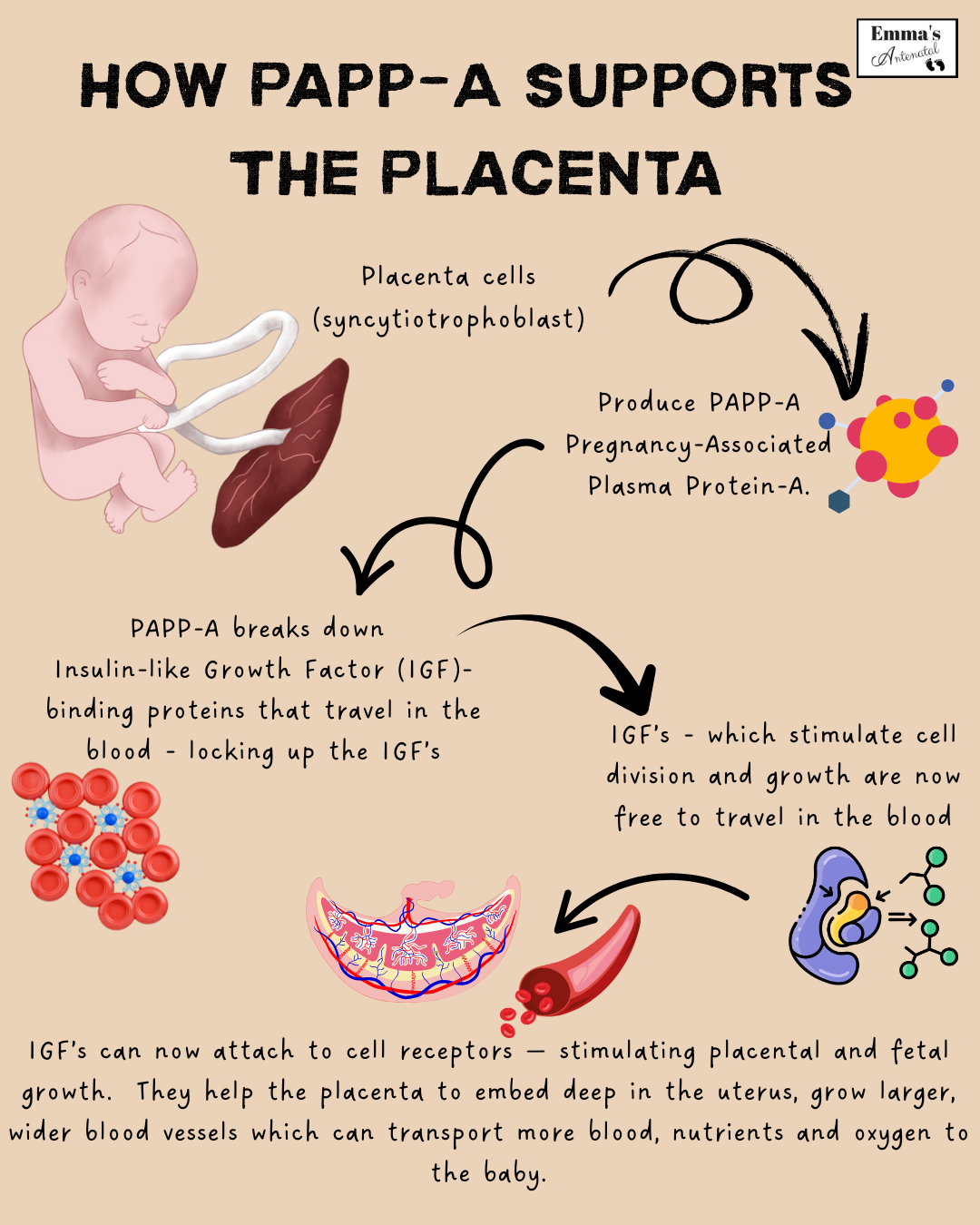
PAPP-A stands for Pregnancy-Associated Plasma Protein-A.
It’s made by the placenta, starting in early pregnancy
and plays an important role in how your baby’s lifeline develops.
It acts like a helper hormone
— regulating the Insulin-Like Growth Factors (IGFs)
that encourage deep placental implantation
and healthy blood flow between mother and baby.
When PAPP-A is lower than average at the end of the first trimester,
it can sometimes signal that the placenta might not be functioning as strongly as usual.
That’s why the NHS usually offers extra monitoring,
and low-dose aspirin
— because that’s what has been studied in large clinical trials.
What’s missing,
sadly,
is any discussion about lifestyle or holistic care.
No one sits down to explain that your own choices
— how you eat, move, rest, and calm your nervous system
— can all profoundly support the health of your placenta going forwards.
🌿 The Evidence for Lifestyle Support
Research into lifestyle factors and placental health is growing,
and it’s painting a clear picture,
which backs up what traditional wisdom knew all along…
the body responds beautifully when nourished,
oxygenated, calm and supported.
So pregnant mama’s are to be treated as goddesses
looked after, pampered with the most nourishing of foods
and given ample opportunity for good exercise and relaxation classes
- such as pregnancy massage and yoga.
Here are my top tips:
A large study found
that women with higher-quality diets in early pregnancy
also had higher PAPP-A and larger, healthier placentas.
A Mediterranean-style diet
— rich in colourful fruit and veg, olive oil, whole grains, nuts, and fish
— has been repeatedly linked with lower rates of
pre-eclampsia, growth restriction, and preterm birth.
Similarly, the Brewer’s Diet,
known for its emphasis on protein,
whole foods, and salt balance,
echoes what the Mediterranean pattern achieves:
stable blood volume, strong blood vessels, and consistent nourishment.
👉🏼 What this means for you:
Eat real, colourful food
— plenty of protein, good fats, bright veg, and minerals.
Avoid: processed seed oils, refined sugars, and highly processed foods that inflame rather than feed.
Every meal is an act of support for your placenta.
Movement feeds your placenta.
When you stretch, breathe, and move gently,
you increase oxygen and blood flow
— delivering more nutrients to your baby.
Several studies have shown that prenatal yoga reduces blood pressure,
lowers stress hormones, and supports vascular function
— all of which improve placental health.
Women who practise yoga regularly in pregnancy also report
fewer complications and a greater sense of connection and calm.
👉🏼 Keep it soft, steady, and regular.
Even a 10-minute daily routine
— hip circles, gentle stretching,
or mindful walking
— keeps the blood and energy flowing.
Yoga Nidra (sometimes called “yogic sleep”)
has been studied for its effects on cortisol
— the main stress hormone that,
when high, can restrict blood flow to the uterus and placenta.
Research shows that regular practice
lowers cortisol,
improves sleep,
and enhances overall wellbeing in pregnancy.
It’s essentially guided rest for your nervous system
— and that rest directly benefits your baby.
👉🏼 Aim to lie down once a day to listen to a Yoga Nidra track
or simply rest your eyes and breathe slowly.
Stillness is productivity when you’re growing a human.
Oxytocin
— the hormone of love and connection —
is a natural antidote to stress.
It opens blood vessels, improves circulation, and keeps the uterus relaxed.
Touch, laughter, safe relationships, and mindful breathing all raise oxytocin naturally.
You don’t need fancy tools
— you need gentleness, safety, and presence.
Your blood volume increases by almost 50% in pregnancy
— your placenta needs every drop.
Stay hydrated with water, coconut water, or herbal teas, and include mineral-rich salts or broths.
This supports blood pressure, circulation, and nutrient delivery to the placenta.
💬 In Summary
Low PAPP-A doesn’t mean your body is broken.
It’s an invitation to slow down and nourish yourself deeply
— physically, emotionally, and spiritually.
While the NHS focuses on clinical monitoring and aspirin
(because those are the interventions that have been studied),
you have powerful, evidence-backed tools at your fingertips:
Eat real, colourful food.
Move gently every day.
Rest and calm your nervous system.
Stay hydrated and connected.
Your body is wise
— it’s communicating, not failing.
Listen, nourish, and trust it. 🌸
📖 Further Reading
A Mediterranean Diet and Risk of Preeclampsia — JAMA Network, 2022
Maternal Diet Quality and PAPP-A Levels in Early Pregnancy — Nutrients, 2020
Yoga in Pregnancy and Its Effects on Maternal Stress and Pregnancy Outcomes — Journal of Obstetric Medicine, 2019
Effects of Yoga Nidra on Cortisol and Anxiety in Pregnancy — Complementary Therapies in Clinical Practice, 2018