RISK RISK RISK? - How Incorrect Assumptions Now Drive Decisions about Women’s Health in Gloucester
Last week, I submitted a detailed Evidence Bundle to the Gloucestershire Health Overview & Scrutiny Committee (HOSC)
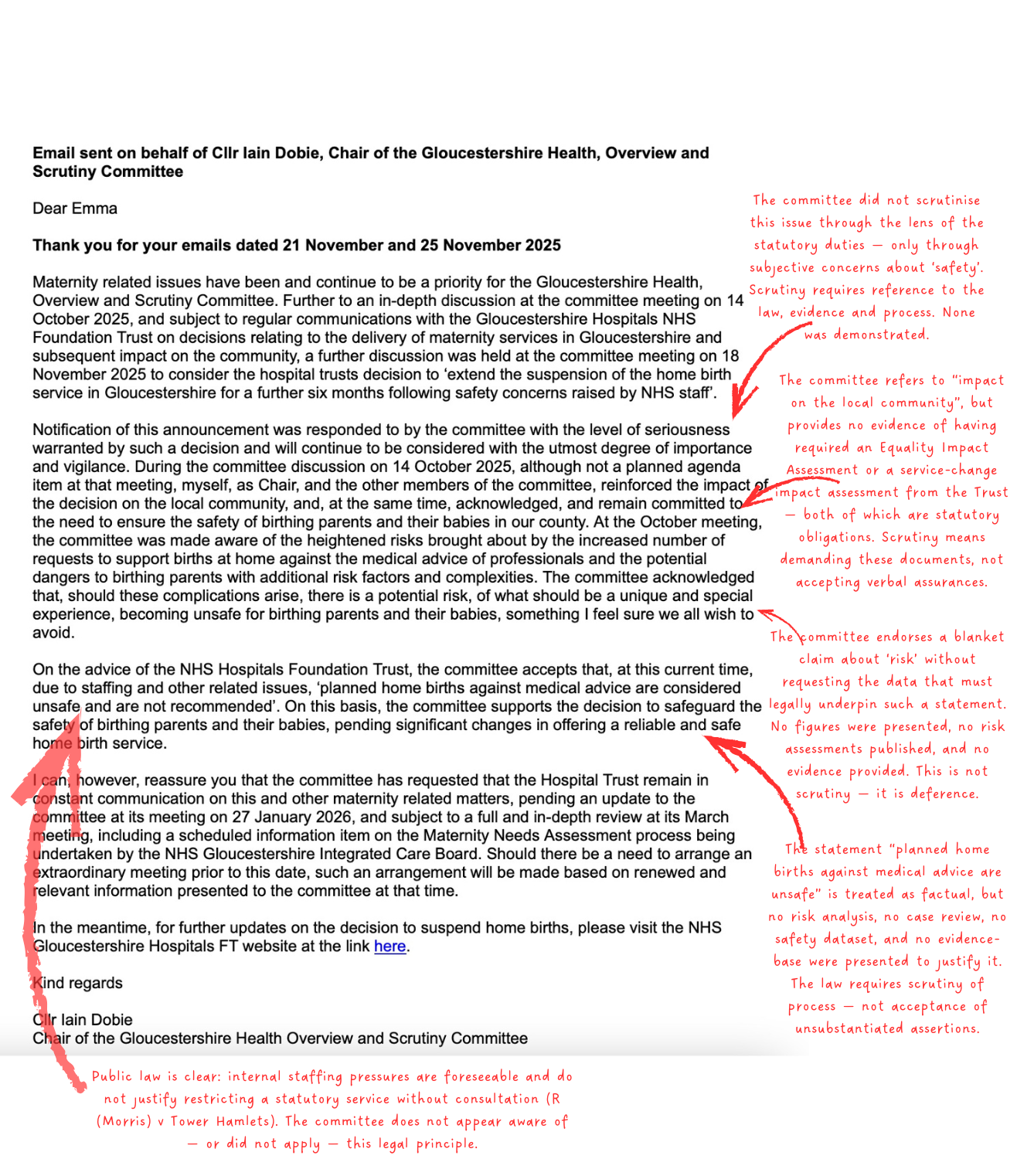
In response, the Chair, Cllr Ian Dobie,
assured me that maternity care is a “priority”.
Watching back the 14 October HOSC meeting
— where CEO Kevin McNamara and Chief Nurse Matt Holdaway presented their maternity update
— something deeply concerning, became obvious.
The entire discussion was built on a single, unexamined assumption:
‘Obstetric = safe, midwife-led = risky.’
This blind belief is now shaping decisions not just inside Gloucestershire Hospitals Trust,
but also inside the democratic scrutiny process that is meant to challenge the Trust
— not echo it.
And because no one is challenging this assumption,
women are losing their legal rights,
their options, and their safest models of care.
How Fear Became “Safety”
When systems are frightened, they retreat to what feels familiar:
• monitors
• machines
• CTGs
• escalation
• “just in case” interventions
In the HOSC meeting, “safety” was repeatedly invoked, but never defined.
No evidence was presented that obstetric pathways are safer than midwife-led care.
No councillor asked for any.
Instead, the assumption stood unquestioned:
❌ More intervention = more safety.
❌ Midwife-led, community care = more risk.
This is the foundational error
now driving the collapse
of Gloucestershire’s midwife-led services.
And it contradicts every major body of evidence we have.
What the Evidence Actually Shows
1. Planned home birth and midwife-led care are as safe or safer
The data is remarkably consistent across decades, countries, and systems:
• Babies do just as well — and in some datasets better — in planned home and midwife-led settings.
• Women have dramatically better outcomes, they have fewer:
– caesareans
– forceps/ventouse
– episiotomies
– infections
– inductions and augmentations
• Women report far higher satisfaction, lower trauma and faster recovery.
(and when we refer to satisfaction - it isn’t that women are putting a fluffy experience over safety.
They mean that they are respected,
and central to decisions and feel things are done with them,
not to them)
Key studies:
• Birthplace in England National Study (2011)
• Cochrane Review: Midwife-Led Continuity Models (Sandall et al., 2016)
• Dutch National Cohort Studies
• Planned Home Birth vs Hospital – multiple international datasets
If you remove medical ideology and looked solely at outcomes,
midwife-led care would be the backbone of Gloucestershire’s maternity system.
2. Continuous CTG monitoring — the symbol of “safety” — has never been shown to improve safety
This matters,
because CTG monitoring is routinely used as the justification for pushing women into obstetric units,
and the Trust repeatedly frames CTG and similar interventions as the solution to “risk”.
But the evidence could not be clearer.
Its has been 40 years since the publication of the landmark Dublin Randomised Controlled Trial
— the biggest and most rigorous CTG study ever conducted.
Study:
MacDonald et al., NEJM 1985
Follow-up: 1989
https://pubmed.ncbi.nlm.nih.gov/3893132/
What did the trial find?
CTG monitoring did not reduce:
• stillbirths
• neonatal deaths
• low Apgar scores
• need for resuscitation
• NICU admission
• long-term developmental problems
Nothing improved.
What did increase?
Caesareans and instrumental births.
In other words:
CTG made outcomes worse for women and didn’t improve them for babies.
This should have ended routine CTG use in the 1980s.
Instead, CTG has been mythologised as “safety equipment”,
and it drives a cascade of unnecessary interventions.
Yet this assumption
— disproven four decades ago —
is still guiding decisions in Gloucestershire today.
3. “Women are more complex, and need more interventions now'“
— a claim with no evidence behind it
Claims about “women being more complex now” are repeated in meetings,
but no evidence has been provided to support them.
Even where some comorbidities are increasing slightly,
this does not justify blanket risk decisions
or funneling women into obstetric care.
-A higher BMI,
-a previous caesarean,
-mild hypertension,
-or being over 35
does not automatically make birth dangerous
— and the research shows many of these women have better outcomes
with continuity-of-carer and midwife-led pathways.
What is driving the rise in interventions is NOT women.
And NOT safety
It is the system.
Unnecessary inductions.
Routine CTG.
Fear-based decision-making.
Loss of continuity.
Defensive practice.
Institutional anxiety.
These are iatrogenic complications
— harms caused by the model of care itself.
Midwife-led models (including home birth) are repeatedly shown to be safe for a broad range of women,
including those with previous caesareans,
when care is relational, continuous and non-interventionist.
Calling women ‘more complex’ while providing no data simply disguises the real source of rising interventions: the culture, practices and fear within obstetric units — not women’s bodies.
4. Caesarean-on-request the real issue:
One councillor asked whether rising caesarean rates are due to maternal request.
This question matters, because:
Many women requesting caesarean do so because of trauma,
fear, or prior poor treatment
— not medical risk.
That could have lead to detailed discussion:
What percentage does this account for of the 50% total caesarean rate?
What support do they receive?
• Could continuity of care reduce this number?
• Could a midwife-led setting keep her emotionally and physically safer?
• Did the system create trauma it is now treating as “complexity”?
But instead, the debate slides into a simplistic binary non-evidence based,
incorrect assumption:
Obstetric = more safety
Midwifery = risky
And women lose access to the very care that would have prevented their trauma in the first place.
And then there’s the part no one talks about: £20 million paid out for birth injury since 2020
Since 2020, Gloucestershire Hospitals NHS Foundation Trust has paid over £20 million in birth injury claims.
These are overwhelmingly cases that occurred under obstetric-led care
— in the very environment being defended as “the safest place”.
If “safety” were really the guiding principle,
we would expect the service with the highest rate of catastrophic harm
— and the highest financial liability
— to be the one under restriction, review or temporary suspension.
But that isn’t what’s happening.
Instead, the safest parts of the system
(home birth, midwife-led units, continuity-based community care)
are being dismantled,
while the part of the system generating the most severe injuries remains unquestioned,
protected, and described as the only “safe” option.
This isn’t evidence-based thinking.
It’s fear-based thinking.
What women need is the right level of care,
chosen with their midwife or obstetrician, based on actual risk
— not assumptions, headlines, or paternalistic narratives about safety.
The Real Problem:
Misunderstanding “Risk”
Risk is NOT reduced by:
• more intervention
• more monitoring
• more hospitalisation
• more CTG
• more escalation
Risk IS reduced by:
• continuity
• listening
• physiological birth support
• autonomous decision-making
• midwife-led care
• homebirth pathways
• calm, low-intervention environments
Every country with world-leading maternity outcomes
— the Netherlands, New Zealand, Iceland, Norway
— builds its system on midwife-led models.
Not because they are ideological.
Because they work.
Why this matters for HOSC
The role of a scrutiny committee is not to absorb the Trust’s worldview.
It is to test it.
❌ Not to sympathise.
✅ To scrutinise.
❌ Not to accept assurances.
✅ To demand evidence.
❌ Not to be guided by fear.
✅ To be guided by law.
At the October meeting,
councillors were given a long presentation, but:
⛔️ no evidence was tested
⛔️ no safety claims were scrutinised
⛔️ no alternatives were explored
⛔️ no documentation was requested
⛔️ no votes or actions were discussed
❌ Scrutiny didn’t happen.
A Q&A session is not scrutiny.
If HOSC continues to operate from unexamined assumptions
— and continues to equate “safety” with “intervention”
— it will continue to make decisions that actively worsen safety for women and babies.
My ask:
If you are on HOSC,
if you work within NHS Gloucestershire,
or represent this county:
Before you make another decision about maternity services,
✅ look at the evidence.
❌ Not the optics.
❌ Not the fear.
❌ Not the defensive instinct to medicalise everything.
👀 Look at the data.
👀 Look at the international comparisons.
👀 Look at the CTG evidence.
🏡 Look at the homebirth data.
🤰🏽 Look at the maternal request research.
🌻 Look at what actually keeps women safe.
Then look at the Law and Legislation
And ask:
Are we making decisions based on evidence —
or based on fear dressed up as safety?
Women deserve a system that knows the difference.
All the evidence, legislation and case law is laid out and indexed in my evidence bundle here.
Please take the time to read and comment below.